NEW YORK (WCBS 880) — A year after the arrival of COVID-19 in America, we know a lot more about the virus, but what remains a bit of a mystery is how and why some coronavirus patients still suffer weeks and months after recovery.
Today, we know it as post-COVID syndrome, and it affects hundreds of thousands, perhaps even millions, of Americans and their families.
By some estimates between 2% to 25% of all COVID survivors have logged some form of post –COVID syndrome symptoms – many for weeks and even months after their recovery.
With so many people reporting symptoms, doctors are beginning to learn more about the mystery of COVID long haulers.
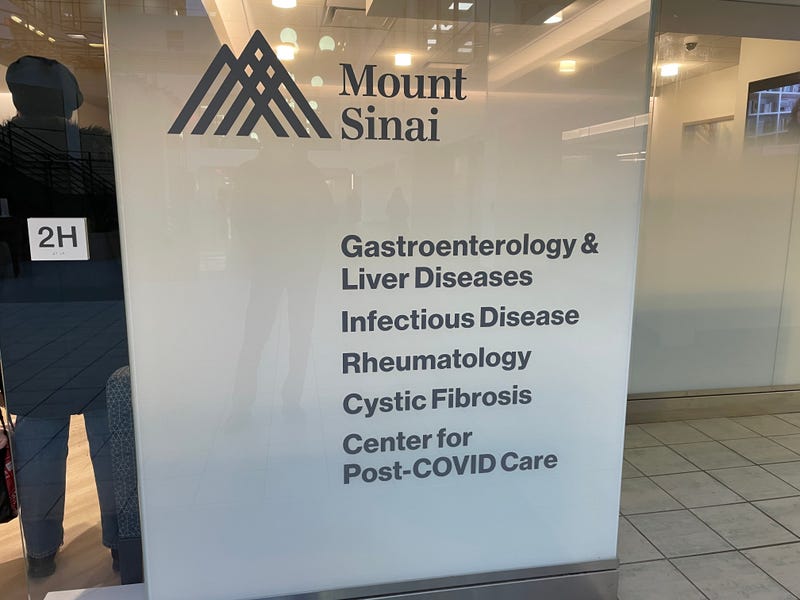
Dr. Joan Bosco, with the Mt. Sinai Hospital Post-COVID Center in Manhattan, said they began seeing patients early last spring when COVID-19 survivors began complaining about significant and nagging post-virus issues. It became a full time specialty for Dr. Bosco and her team.
“I guess just seeing more patients, and learning more about patterns and similarities amongst patients, did help us to sort of narrow our focus in a way but, I think there’s still a lot to be learned,” Bosco said. “We’ve been seeing a lot of interesting symptoms post-COVID that we originally didn’t necessarily know were associated with the post-COVID syndrome and every time I meet a patient I learn something new.”
While there appears to be an overall trend of symptoms, Bosco said everyone seems to exhibit their own “unique flavor” of post-COVID syndrome.
Some involved in the research experience mild to no symptoms while others suffer from fatigue, dysautonomia, brain fog, neuropathy, anxiety and depression.
Bosco said they focus on treating and managing symptoms and also offer rehab programs to treat fatigue and dysautonomia to help build a patient’s stamina and strength.
Since opening the center, they have treated 1,800 patients and are now talking about opening up new facilities to help with the demand. They’re taking appointments today for August.
We spent time with Dr. Bosco at the Mt. Sinai Center for this week’s In Depth Podcast and one of the most interesting things she told us was that this post-COVID condition isn’t as surprising as some may think.
“We have seen this before with other viruses. I think the difference here is that it’s just on such a larger scale. At least in New York, everyone got sick in March and April, everyone’s having their post-COVID symptoms at the same time,” Bosco said.
Mount Sinai is trying to figure out why some patients continue to experience symptoms long after recovery while others appear to get better without having to look back.
“We’re trying to see if there are any trends to this,” Bosco said. “It’s not necessarily the patients who had the most severe acute illness who have the most severe post-COVID symptoms so, that’s another thing we’re trying to figure out. Why are the more milder initial cases having significant post-COVID symptoms?”
At this point, Bosco said they’re still in the data collection stage.
“From my anecdotal experience seeing patients I personally haven’t noticed any trends. It seems like young, healthy patients are affected, older patients are affected,” Bosco said. “I like to tell patients, ‘This is what we can expect, this is what we’ve seen.’ So, it is a little frustrating when we don’t have a clear course that we can lay out for patients.”
She is hopeful that the majority of post-COVID patients will recover.
“I do think the majority are going to get better. It is a slow gradual process, we’re now a year out from when most patients got sick in New York last March and our center is clearly still full, so certainly patients are still symptomatic a year out, but the overall trend is that they are getting better and I do think this will be, for a majority of the patients, a transient process,” Bosco said.

One of the patients Dr. Bosco saw this week is Caitlin Barber.
Her story offers hope for COVID long-haulers who don’t yet see an end to their nightmare.
Barber was a healthy 27-year-old when she caught the virus last March, likely from the nursing home she worked at as a dietitian.
Barber got better within a few weeks, but then got leveled by wave after wave of post-COVID syndrome symptoms.
“My initial COVID wasn’t too bad and the post-COVID symptoms started right when I tried to go back to work post-COVID,” Barber said.
When she first got sick, Barber said she was tried and experience headaches and body aches, but her symptoms grew progressively worse for the next six months.
“I was exhausted to the point where I couldn’t get off the couch and that was the biggest issue along with the body aches, the headache, the dizziness, the loss of taste and smell, the mind fog, there were dozens of symptoms that just kind of came in waves and a lot of it was just trying to manage each individual symptom until I could get the proper help,” Barber said.
Worse than that, many of the health care professionals she sought answers from doubted her story. They simply couldn’t understand what was happening to this healthy 27-year-old.
“My doctors at home said it was all in my head,” Barber said. “They told me to ride it out and we were hoping it would just go away and unfortunately, that wasn’t the case.”
Barber felt like all hope was lost.
“It was terrible,” she said. “I cried myself to sleep every night. I knew that there was something wrong. I was not right. I was like an Energizer bunny, I was constantly moving and now I can’t get off the couch.”
By the fall, Barber couldn’t even walk. She and her husband were forced to move out of their apartment and live with her in-laws.
“I couldn’t stand up, I couldn’t move my arms, my husband was carrying me to the bathroom. At one point, I needed three people to shower me. I couldn’t even stand up on my own without my heart rate going off the charts so physically, to be so debilitated when you were so free before, you feel like you’re trapped in your body,” Barber said.
It wasn’t until she got into Mount Sinai’s Post-COVID Center that things started to turn around.
Doctors put her on a personalized program to put her on the road to recovery that included breath work, physical therapy, compression stockings, and other treatments.
“So now I am feeling pretty good. It’s been almost a year of my COVID journey and it’s been quite a year but, I am slowly recovering and making a lot of progress,” Barber said. “My husband and I, we went many, many months without hope that I would ever get better. COVID really took my body and did a number on it and it’s a very hard virus to deal with and a lot of odds were against me. I was pretty much bed-bound at the worst, I needed three people to shower me. So the odds were against me but I have incredible medical providers down here in New York City and that’s why I’m better.”
But the journey was long, and sometimes very dark.
“It was scary, it was frustrating. We had a front row seat and lived the COVID-19 pandemic unexpectedly,” her husband, David, said. “We figured that one of us would probably get it but, we had no idea that it would go on for almost a full year. It’s truly life changing for us.”

This week, Barber marked a major milestone in her recovery. For the first time since receiving treatment, she was able to walk into the Mount Sinai Post-COVID Center.
“Last time I was at the Post-COVID Center was about December and every time I’ve come here I’ve been in a wheelchair so finally, after a year, to be able to walk in felt so good. It’s an amazing feeling,” she said.
In addition to her treatment, Barber has joined a Facebook support group called Survivor Corps, which bills itself as a “grassroots movement educating and mobilizing COVID-19 survivors and connecting them with the medical, scientific and academic research community, to help stem the tide of this pandemic and assist in the national recovery.”
“There’s a lot of long haulers out there who are really suffering and I hope to be the hope for them,” Barber said. “I hope to be someone they can look at and say, ‘Okay, this is possible, we can get better.’”
LISTEN NOW on the RADIO.COM App
Follow WCBS Newsradio 880
Facebook | Twitter | Instagram
