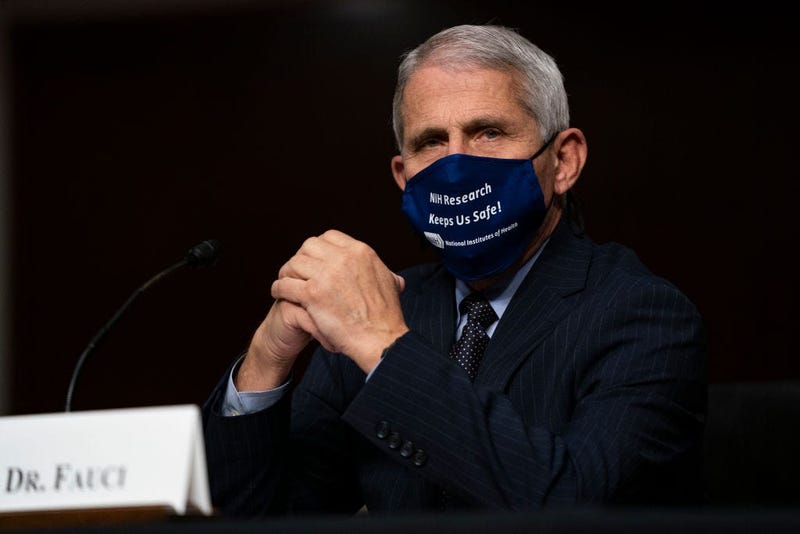
Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, told military and veteran caregivers that the United States may have a "very difficult fall and winter" because of the pandemic.
Fauci spoke during the Elizabeth Dole Foundation's fifth annual National Convening event on Monday, joining remotely by video call. He gave a presentation on the public health and scientific challenges of "this historic COVID-19 pandemic."
The novel coronavirus, or SARS-CoV-2, which causes the COVID-19 disease, "has exploded upon our world as the most extraordinary and impactful pandemic in the last 102 years, ever since the famous 1918 swine flu" with more than 38 million cases worldwide and more than 1 million deaths. The United States has been hit hardest, with nearly 8 million cases and more than 215,000 deaths as of Oct. 14.
As the season turns, Fauci said Europe is now facing a strong spike in cases of the coronavirus. The United States peaked earlier this summer, saw a lull in September, but is also surging again.
"This looks like we're going to have a very difficult fall and winter," he said.
The virus is primarily transmitted through respiratory droplets when close to an infected person, or particles that remain in the air over time and distances, especially in closed-air environments. Less commonly, it can be transmitted through contact with contaminated surfaces. The virus is also found in a variety of body fluids and secretions, though Fauci said its still uncertain, but unlikely that those are major sources of transmission.
The highest risk for airborne transmission includes crowded, enclosed spaces with poor ventilation and people singing, speaking loudly or breathing heavily without personal protective gear such as masks. Most transmission happens in households, or in areas people gather that lack ventilation and where people are not wearing masks.
"You don't need to be coughing or sneezing to transmit the infection," he said.
One of the most distinctive things about COVID-19 compared to other viral infections, is that about 40-45% of people are asymptomatic, Fauci said, but modeling studies show "a substantial portion of the transmissions occurs from someone who is without symptoms to an uninfected person." People without symptoms could account for as more than 50% of infections, according to those studies, he said.
The fundamental ways to prevent infection or spreading the virus include universal wearing of masks or cloth face coverings, physical distancing of at least six feet, frequent handwashing, avoiding crowds or "congregate settings," and outdoor settings are "always safer" than indoors.
"I have repeated this many times public, but I think it's worth repeating now," he said.
The four types of coronavirus are responsible for about 15-30% of the "common colds" people experience, Fauci said, though most are "relatively benign."
He walked the audience through the history of coronavirus during pandemics, from the SARS pandemic in 2002 to the MERS pandemic of 2012, both caused by transmission from animals to humans, to the current pandemic.
The COVID-19 disease manifests as a flu-like syndrome "early on," Fauci said, with most patients experiencing fever, cough, fatigue, loss of appetite, shortness of breath and other symptoms. But some patients experience loss of taste or smell ahead of respiratory symptoms.
Up to 81% of symptoms from the virus are "mild to moderate" and "don't require special medical intervention such as hospitalization," Fauci said, while 19-20% of cases have "severe to critical" symptoms. People with severe COVID-19 may experience neurological disorders, acute respiratory distress, hyper-inflammation, heart dysfunction, acute kidney injury, multisystem inflammatory syndrome in children and more.
"As we learn more and more about this disease and its manifestations, we see that other organ systems, particularly the heart (are affected)," he said, including cardiomyopathy, arrhythmias and other issues that can sometimes "lead to sudden death" as well as neurological issues or blood clot issues that can lead to strokes in "otherwise normal individuals."
People at highest risk are still older people or those of any age with underlying conditions such as obesity, diabetes, heart conditions and for smokers.
"Younger people clearly do not get as many of the clinical manifestations ... that make them severely ill," he said, compared to much older individuals, especially those 65 and older.
Many veterans are older or have conditions that place them at higher risk, including specific military toxic exposures that may make them particularly vulnerable. Veterans of different races or ethnicities may also face higher risk.
"One of the characteristics of this disease that's most disturbing is the extraordinary racial and ethnic disparity," Fauci said. Minorities in the United States, especially Black, Latino, Native American, Native Alaskan and Pacific Islander populations.
Those groups have a higher risk of getting infected because they often hold jobs with high exposure risk "on the frontline in the community." But those groups also often have higher risk of comorbidities that can lead to worse COVID-19 symptoms. Hospitalization rates for those groups are also often significantly higher, on average.
That data is born out at the Department of Veterans Affairs, where data and studies show that Black and Hispanic veterans make up nearly half of all VA COVID-19 cases, though they account for only 23% of all VA patients. Black and Hispanic veterans are also twice as likely to test positive for COVID-19 than white veterans.
Fauci mentioned the treatments being tested, including antiviral medications and convalescent plasma, as well as the vaccines currently being developed. He said the hope is to prioritize the first rounds of the vaccine for those most at risk, including healthcare workers and those with underlying conditions.
—
Veterans exposed to burn pits could be at higher risk for COVID-19
Some Gulf War veterans could be at higher risk for COVID-19, expert says
Black, Hispanic veterans twice as likely as white vets to test positive for COVID-19, VA study finds
About 17 VA patients have died of COVID-19 daily since the first veteran death 7 months ago
