Jimmy Arocho was an Army sergeant first class. He worked battlefield surveillance and intelligence support. He tried to take care of himself -- he didn’t smoke, exercised regularly, watched what he ate, tried to get enough sleep. But he felt awful.
He just couldn’t figure it out.
His whole body hurt, he was chronically tired, had trouble focusing and a litany of other problems. And over time, he began to lose his edge. The writing was suddenly on the wall when an Army doctor told him the VA would be able to help him. He hadn’t even retired yet.
“It was a career-ender already,” he said. “You could just tell.”
A team of Florida Department of Veterans Affairs doctors couldn’t come up with the answer to his problems. Then, things took a sharp turn.
Driving to work one day, Arocho fell asleep behind the wheel of his car.
“It scared me,” he said. “I knew then something was really, really wrong.”
It didn’t get better. Arocho found himself having to get special exceptions at work for what he thought was narcolepsy. Driving had become a significant safety risk.
“I couldn’t function like a normal person,” he said. “And I -- and this VA team -- couldn’t figure out why.”
It took several rounds of specialty care appointments, studies and tests before doctors began to put their finger on it.
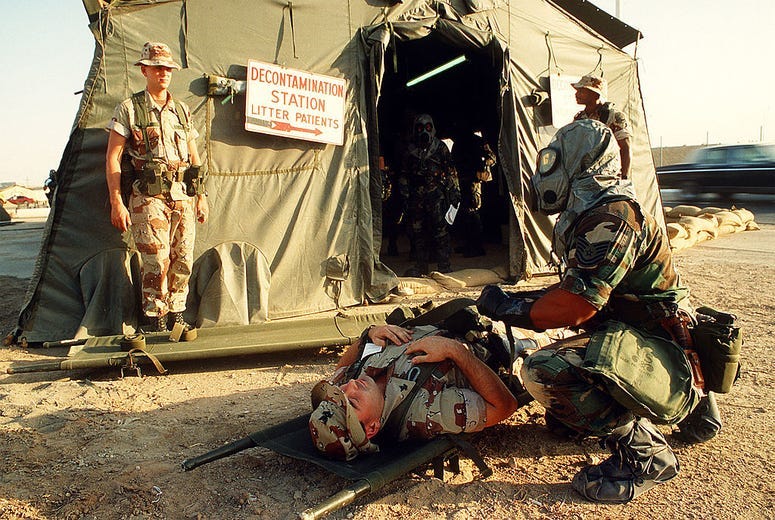
Arocho served in the Gulf. Working in battleground surveillance, he had been exposed to toxins from demolished captured munitions, including nerve agent sarin.
“The alarms went off, we wore the charcoal suits and the rubber masks” Arocho remembers. “But nobody knew how bad it could be. That downwind environment … we had no idea how bad it would be.”
Connecting his illnesses to his service was revelatory for Arocho. But it wasn’t exactly encouraging.
“I look out my rearview mirror on toxic exposure and what do I see? Vietnam vets still struggling to get help for Agent Orange,” he said. “This has been happening for the last half-century. It’s not a mystery what happens when we go around the world fighting these wars. We’re exposed to things that come back to bite us.”
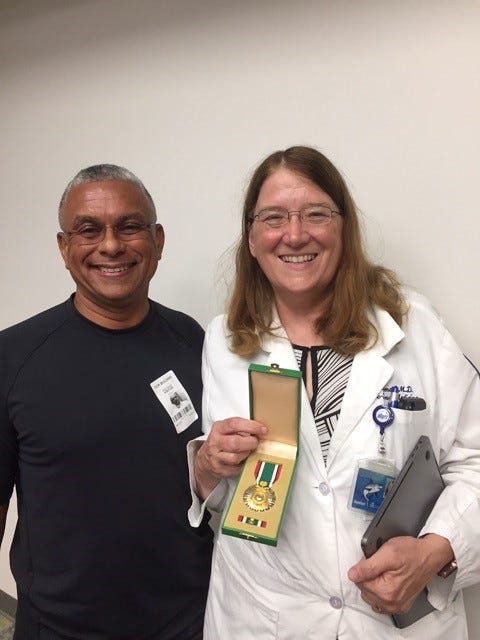
Once there was a theory, a thread of evidence that could connect his service to the health issues he was suffering, Arocho found Dr. Nancy Klimas, a VA physician and director of the Institute for Neuro-Immune Medicine at Nova Southeastern University. Klimas is an expert in what researchers call Gulf War Illness and she needed his help, too.

What is Gulf War Illness?
The first Gulf War in 1991 likely exposed service members to the highest level of toxins since World War I, Klimas told Connecting Vets.
“It was really intense,” she said.
Troops were exposed to nerve agent sarin, organic phosphate, oil-well fires, burn pits, anthrax vaccines and uniforms “impregnated with pesticides,” among others.
“It was one thing after another,” Klimas said.
Scientists don’t know precisely which of those many toxins were actually responsible for what researchers now see as Gulf War Illness (GWI), though it’s not yet a formal medical diagnosis.
“It might have just been the perfect storm of all those things,” Klimas said.
Today, one in three veterans who deployed in the first Gulf War is sick.
“It’s an enormous number of ill people and many of them are disabled,” she said.
Klimas runs a small VA clinic devoted to GWI veterans, though most of her time is taken up in researching a cure.
In the past 10 years -- particularly the last five -- Klimas said veterans advocates and service organizations are responsible for “kicking a lot of funding out of Congress” for research into GWI.
The scientific progress “has been huge,” she said, including a much better understanding of GWI as “an illness that started with neurotoxin exposures and created a chronic brain disease that is a neuroinflammatory and oxidative stress combination of things happening in the brain that cause a lot of different systems in the body to be affected,” Klimas said.
When the brain is affected in this way, the systems the brain regulates -- including endocrine, autonomic and immune systems -- can become “out of balance,” she said, “resulting in an illness that includes a lot of pain, cognitive dysfunction, irritable bowel” and a “tremendous shopping list of symptoms.”

What happens now?
Now that there is a much better understanding of what GWI is, Klimas said her team and others have been funded by VA and the Pentagon to finally conduct clinical trials for possible treatments, including medication.
“We need to somehow connect to veterans to let them know,” Klimas said. “Many of them feel very discouraged. They may have come to the VA early on when they were first ill and found that we didn’t know how to help them and they just left or they might not even have VA privileges and they’re seeing civilian doctors and they know nothing about Gulf War Illness.”
Many may not even be diagnosed, Klimas said, since GWI is not an official diagnosis code even within VA. Instead, veterans can be diagnosed with multiple symptom illnesses that include irritable bowel, fibromyalgia and other full-body chronic pain and chronic fatigue. Symptoms can include fatigue, poor sleep, pain, gastrointestinal issues, problems with concentration and attention and more.
“We want to share this message of hope that this progress has been galloping and after years of frustration,” she said. “We’re finally figuring it out.”
Klimas and her team at the Miami VA and INIM turned a pivotal corner in being able to conduct their clinical trials. Now, if they can get the veterans to participate -- healthy and ill -- they can test a series of several medications that supercomputer monitoring and animal testing shows could possibly cure GWI by “rebooting” those unbalanced systems in the body.
“It’s a moonshot, but the good news is there’s hope,” she said. “We’re doing kickass science but nobody knows. We have our shoulder to the boulder, pushing it along. We’ve been at this a long time and we just need help getting it done ... We believe we're close to a potential cure."
Klimas and her team estimate as many as 300,000 veterans have GWI, but they’re hard to pin down.
“It sounds like a lot and that you could go out and do studies, but if they’re not in a VA already, it’s really hard to reach them,” she said. “Most of our trials are so slow because we can’t find the vets to recruit into our studies. Some of these have been dragging out for years -- even simple studies.”
While she’s anxious to complete the trials and move forward, Klimas said it’s often fear that drives her.
“My biggest paranoia about Gulf War Illness, my most front-burner, scared, please-let’s-get-this-done-right hurry is that when the brain is under these conditions and the population is aging, these people are at risk for neurodegenerative disorders” such as Parkinson’s disease, she said.
“We have to intervene now and not wait and see who’s gotten even more sick 10 years from now because we didn’t get stuff done in a timely way.”
Recruitment is all that’s standing in her team’s way.
“It’s not the science, we have the science. It’s not the money, we have the money” -- $20 million, in fact. “Where are the friggin’ patients? That’s what’s stopping us.”
That’s where Arocho, now retired and 62, comes in. He specializes in outreach to veterans struggling just like he was.
“So many of us struggle in the same ways -- we go in and get handed meds like ‘take these pills, go home, get a life,’” Arocho said. “It’s easy to get frustrated, to lose hope. To this day, we deal with the same bullshit. And it’s on our faces, we can recognize each other when we’re having a hard time when our doctors are telling us we’re crazy. Sometimes you just need someone you know will understand. That’s what I try to do.”
Some of Klimas’ clinical trials can be conducted at a distance -- far from Klimas’ home base at the Miami VA and the INIM -- online, over the phone and by mail.
The main qualification? You have to have been deployed in the Gulf War in 1991 -- but you don’t have to be sick.
“You can go into combat knowing that you might lose your leg, and if you did, you would go to Walter Reed and you would get a prosthetic and someone would teach you to walk again,” Klimas said. “But it’s awful hard I think for folks to see the effects of these hidden toxins they don’t even know they’re breathing in … that will come back and snap you later in life and that we’re not ready to help them. We want to -- we need to -- do that.”
"We want them to know there's hope," Arocho said. "There are people here who understand. We're here to help."
Join the research
For more general information, call 305-575-7648 or email VHAMIAGWI@va.gov.
For information about the clinical trials, call 954-262-2870 or email ZKirby@nova.edu.
For more on the different studies Klimas and her team are working on, click here.
To participate in their GWI online survey, click here.
-