SAN FRANCISCO (KCBS RADIO) – June 19th is not only Juneteenth, it is also World Sickle Cell Awareness Day.
“Sickle cell disease affects about 100,000 people in the U.S.,” UCSF psychologist Marsha Treadwell, PhD, told KCBS’ Bret Burkhart on this week’s episode of As Prescribed. “They're primarily blacks and African-Americans, although there are also many people of Latinate background who are affected. And it is a genetically transmitted condition, so both parents have to have the trait.”
Treadwell’s special focus is on patients with sickle cell disease at UCSF’s Comprehensive Sickle Cell Center at UCSF Benioff Children’s Hospital Oakland.
She said when both parents have the trait, there is a 25 percent chance that the child will have sickle cell disease. However, both parents must have the trait – not one or the other.
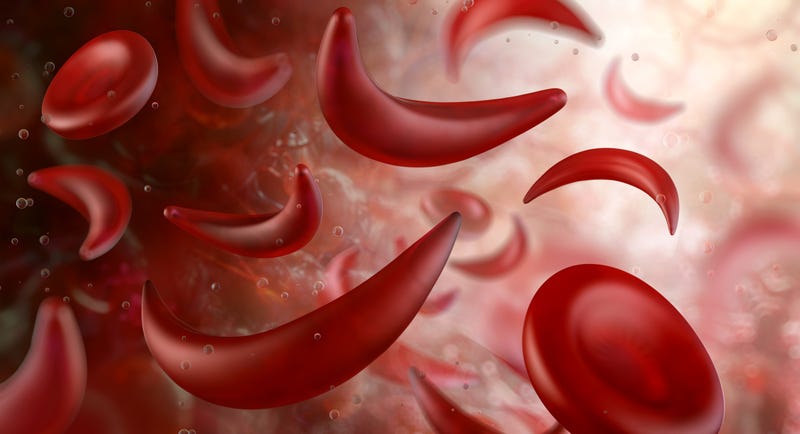
“The disease affects every possible organ system because it affects everywhere that blood flows. So you can have brain problems, eye problems, and sickling in the lungs. It's a very complex disease.”
The reason some populations are more prone to sickle cell disease is because of humanity’s history with malaria.
“There's a belt around the world where malaria had been endemic and the sickle cell trait actually served as protection against malaria,” Treadwell explained. “But then, when the child inherited the two traits from both parents, they ended up with sickle cell disease, which in and of itself is again life threatening and doesn't itself protect against malaria. But that's why it primarily arose in Africa.”
She also noted that there is a similar population in southeast Asia for the same reason.
The slave trade then made sickle cell disease common in Brazil and the southeast portion of the United States.
In the San Francisco Bay Area, the UCSF Comprehensive Sickle Cell Center has been treating patients with the disease for more than 50 years.
“It's very interesting that it began in relationship to a community partnership between the Black Panther Party and community providers who started really working with people with sickle cell disease and sickle cell trait,” said Treadwell. “And from there, advocacy led to legislation where the first comprehensive sickle cell centers were funded by the US government at the time.”
She said this center not only handles the physical aspects of the disease and all of the challenges that come with it – but also works on the psychological wellbeing of patients and their quality of life.
“The overall quality of life can be very much devastated as they face uncertainty related to their disease process, concerns about their own mortality and grief and loss as they lose friends and loved ones,” the psychologist added.
Part of that involves the mindset patients have in the process.
“More and more are embracing being called warriors,” Treadwell shared. “And I think that's so fitting because what comes with this legacy of being black or African American – primarily in the United States – is stigmatization, discrimination, accusations related to being drug seeking when people are seeking relief from their pain. And really dealing with multiple medical traumas from a very early age.”
She noted that complications from sickle cell disease can start from infanthood and continue through adulthood.
“So it does take a warrior to be able to manage in the face of severe complications, severe pain, medical traumas with multiple procedures, and then a community that isn't always embracing and in fact can be stigmatizing.”
But, the future for people with sickle cell disease may be brighter.
Treadwell said bone marrow transplantation and stem cell transplantation – first done at Zuckerberg San Francisco General Hospital and Trauma Center decades ago – have been proven to cure the disease.
However, there are limitations.
“It's not available to the majority of patients,” Treadwell explained. “You have to have a matched donor and there are risks that come with the cure. So there's what's called a conditioning regimen where your body has to be made able to accept these stem cells that belonged to someone who's your match. That can in itself create some life threatening situations. And then the graft can be rejected.”
A different treatment plan is currently being researched.
Treadwell said UCSF’s hematology division chief Dr. Mark Walters is currently gene editing therapies to treat sickle cell disease.
“Dr. Walters received the largest grant in the Benioff Children's Hospital's Oakland history for his gene editing trials,” she continued. “And what happens here is that the individual's own cells are edited and then they're reintroduced back into the person's body. The hope, and it often happens, is that they grow into healthy cells that don't have sickling.”
She said it would be a game changer for curing sickle cell disease since it would eliminate the complications and challenges many bone marrow or stem cell transplant patients deal with and offer a solution that is a perfect fit for each patient.
That research is currently in the trial stage.
